Top 10 Publikationen
Krone L, Mahankali S, Geiger T. Cytolysin A is an intracellularly induced and secreted cytotoxin of typhoidal Salmonella. Nat Commun. 2024 Sep 28;15(1):8414. doi: 10.1038/s41467-024-52745-0. PMID: 39341826
Krone L, Faass L, Hauke M, Josenhans C, Geiger T. Chitinase A, a tightly regulated virulence factor of Salmonella enterica serovar Typhimurium, is actively secreted by a Type 10 Secretion System.
PLoS Pathog. 2023 Apr 5;19(4):e1011306. doi: 10.1371/journal.ppat.1011306. eCollection 2023 Apr. PMID: 37018381
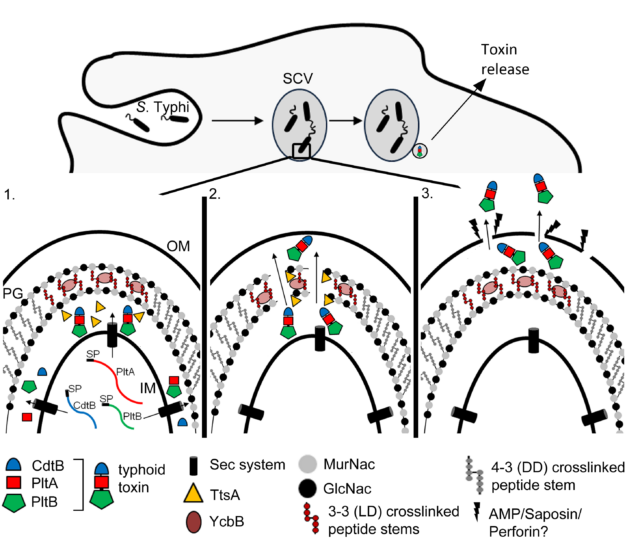
Geiger T, Lara-Tejero M, Xiong Y, Galán JE. Mechanisms of substrate recognition by a typhoid toxin secretion-associated muramidase. Elife. 2020;9:e53473. Published 2020 Jan 20. doi:10.7554/eLife.53473.
Geiger T , Pazos M , Lara-Tejero M , Vollmer W, Galán JE. Peptidoglycan editing by a specific LD-transpeptidase controls the muramidase-dependent secretion of typhoid toxin. Nature Microbiology, 2018 Nov;3(11):1243-1254. doi:10.1038/s41564-018-0248-x
Gratani FL, Horvatek P, Geiger T, Borisova M, Mayer C, Grin I, Wagner S, Steinchen W, Bange G, Velic A, Maček B, Wolz C. Regulation of the opposing (p)ppGpp synthetase and hydrolase activities in a bifunctional RelA/SpoT homologue from Staphylococcus aureus. PLOS Genetics. 2018 Jul 9;14(7)
Münzenmayer L, Geiger T, Daiber E, Schulte B, Autenrieth SE, Fraunholz M, Wolz C. Influence of Sae-regulated and Agr-regulated factors on the escape of Staphylococcus aureus from human macrophages. Cellular Microbiology. 2016 Aug;18(8)
George SE, Nguyen T, Geiger T, Weidenmaier C, Lee J, Liese J, Wolz C. Phenotypic heterogeneity and temporal expression of the capsular polysaccharide in Staphylococcus aureus. Molecular Microbiology. 2015 Dec;98(6):1073-88.
Grosz M, Kolter J, Paprotka K, Winkler AC, Schäfer D, Chatterjee SS, Geiger T, Wolz C, Ohlsen K, Otto M, Rudel T, Sinha B, Fraunholz M. Cytoplasmic replication of Staphylococcus aureus upon phagosomal escape triggered by phenol-soluble modulin α. Cellular Microbiology. 2014 Apr;16(4).
Geiger T, Kästle B, Gratani FL, Goerke C, Wolz C. Two Small (p)ppGpp Synthases in Staphylococcus aureus Mediate Tolerance against Cell Envelope Stress Conditions. Journal of Bacteriology. 2014 Feb;196(4):894-902.
Geiger T, Francois P, Liebere M, Fraunholz M, Goerke C, Krismer B, Schrenzel J, Lalk M, Wolz C. The Stringent Response of Staphylococcus aureus and its impact on survival after phagocytosis through the induction of intracellular PSMs expression. PLOS Pathogens. 2012 Nov; 8(11).